Do you know that feeling when your legs are heavy and tired in the evening? Or the slight aches and pains and the unpleasant tingling sensation that sets in after a long walk or sitting for a long time? For many people, these discomforts are part of everyday life and are therefore often dismissed as normal signs of fatigue. But these symptoms can also be caused by varicose veins – a common venous condition that is not only visually disturbing but can also pose a health risk.
In the following article, we would like to explain in detail all aspects of the condition varicose veins (varicose veins). Here, you'll learn everything you need to know about their development, the appropriate treatment, and, above all, we'll provide you with numerous tips for prevention.
Let's start with the most important question: What are varicose veins? Varicose veins, also known as varicosities, are enlarged, swollen, and twisted veins visible beneath the skin's surface. They commonly occur on the legs, but can also occur elsewhere in the body. The cause is a weakness in the vein walls and valves, which impairs blood flow to the heart and leads to blood pooling in the veins.
Content
1. A first overview: What different types of varicose veins are there?
2. These varicose vein symptoms may occur
3. Are varicose veins dangerous?
4. This is the number 1 cause of varicose veins
5. You should consider the following risk factors
6. Treat varicose veins - effectively & painlessly
7. Relieve varicose veins with acupressure
8. When is varicose vein surgery advisable?
9. How to prevent varicose veins
An initial overview: What are the different types of varicose veins?
Medically, the veins in the legs are divided into the superficial and deep venous systems. The veins located deep within the body carry approximately 90 percent of the venous blood in the legs back to the heart. In contrast, the superficial veins are located directly beneath the skin. There are four types of varicose veins within the superficial venous system.
Spider veins are the mildest form and appear as delicate reddish or bluish varicose veins on the skin. Although they are usually painless, they can be cosmetically disturbing and affect self-confidence.
Reticular veins are located directly beneath the skin in what are known as reticular veins. As their name suggests, they are thin, arranged in a network-like pattern, and are approximately one to three millimeters thick. They are often cosmetically disturbing but rarely cause pain or other discomfort.
Side branch varicose veins can be either congenital or caused by chronic venous congestion. They often occur on the sides of the legs and can become quite painful with prolonged standing or sitting.
Truncal varicose veins develop in the large saphenous veins, often as a result of a congenital defect in the venous valves. These varicose veins are particularly visible and can cause significant discomfort such as pain and swelling.
These varicose vein symptoms can occur
Now that we know more about the question "What are varicose veins?" we can focus on the signs of varicose veins. Varicose veins most commonly occur on the legs. Symptoms range from visible, swollen veins to pain, heaviness, and swelling. Itching or a burning sensation around the affected veins, as well as skin changes (discoloration or hardening), and muscle cramps, especially at night, are also common.
Varicose veins in the thigh tend to be particularly painful, as they are often accompanied by a pulling sensation. These symptoms can be aggravated by prolonged standing or sitting and therefore usually worsen over the course of the day. Many sufferers are particularly affected on hot days and experience a significant reduction in their quality of life. This is also due to the fact that varicose veins not only cause pain but are also unfortunately very noticeable.
By the way: Varicose veins in the feet are also not uncommon. There, they usually cause similar symptoms to those in the legs: the feet can swell and become painful, especially after prolonged standing or walking. Visible veins in the feet are often an indication of venous insufficiency, which originates higher up in the legs.
Are varicose veins dangerous?
Now let's get to the proper diagnosis and treatment. You may be wondering: Varicose veins - which doctor can help me? Or: How dangerous are my varicose veins?
In most cases, varicose veins are not life-threatening, but they can lead to serious complications if left untreated. Therefore, if you suspect you have varicose veins, you should consult a vascular surgeon or phlebologist. These specialists can provide an accurate diagnosis and recommend appropriate treatment options. If varicose veins are left untreated, complications can arise, especially in advanced stages. For example, the increased pressure in the veins may cause fluid to leak into the leg tissue. This can result in swelling, known as edema. Additionally, red blood cells can enter the tissue, causing reddish-brown skin changes on the legs.
Changes in the vessel walls and reduced blood flow velocity can also cause inflammation in the varicose veins (varicophlebitis), which is accompanied by the formation of blood clots (thrombi). Ulcers on the lower leg, known as leg ulcers or leg ulcers, can also develop over time if varicose veins are left untreated.
In rare cases, varicose veins can even burst (varicose vein rupture) and cause heavy bleeding. Immediate first aid measures are then required, such as calling emergency services, elevating the leg, and applying a bandage. As you can see, we cannot ignore this issue; we should act as soon as possible. So that you can take appropriate measures for treatment and—even better—prevention, we will now explain the causes in detail.
This is the number 1 cause of varicose veins
We'd like to get to the bottom of the question "How do varicose veins develop?" To do so, we'd like to give you a little background information so you're fully informed: The medical term for varicose veins is varicose veins. This term is used to describe diseased, enlarged veins that result from venous valve insufficiency.
When we talk about varicose veins in connection with varicose veins, we mean the complete clinical picture, including symptoms, causes, and treatment options. This encompasses the entire spectrum of the disease and its effects on the body. The main cause of varicose veins is a weakness of the vein walls and valves. This weakness can be genetic or exacerbated by prolonged standing or sitting, obesity, pregnancy, or hormonal changes.
Varicose veins develop due to a malfunction of the venous valves. These valves normally prevent blood from flowing backward and pooling in the veins. If the valves don't close properly, blood collects in the veins, causing them to dilate and deform.
You should consider the following risk factors
With this knowledge, it's easy to identify some risk factors for varicose veins, such as anything that impedes the return of blood from the legs. These include tight clothing, pregnancy (weight gain and hormonal changes), sports that require abdominal exercises, heavy lifting, chronic coughing or constipation, which causes straining and a strong recoil in the leg veins, prolonged sitting or crossing the legs, and being overweight.
Factors that weaken vein walls also contribute to the development of varicose veins. These include hormones such as those found in the pill, menopausal hormones, and during pregnancy, alcohol consumption, and heat exposure, such as saunas, hot baths, or underfloor heating. There are also factors that impede or deactivate muscle pumping, such as prolonged standing or sitting, wearing high heels, and paralysis.
Also important to note: Venous diseases can also be hereditary. So if members of your family already exhibit similar symptoms, it's likely that you could be affected as well.
Treating varicose veins – effectively & painlessly
Now let's get to the point: What helps against varicose veins? And is it even possible to reverse them? There are various options for treating varicose veins. These include sclerotherapy, laser treatments, and minimally invasive surgical procedures, which we will discuss in more detail later.
Conservative treatments and certain behavioral measures can also help against varicose veins. Special medications, including those made from natural extracts, can be used as complementary therapy, primarily to support the strength of the vein walls. Here's an overview of the most important treatment options:
- Medical compression stockings: Basic treatment for varicose veins combines wearing medical compression stockings with regular exercise. These stockings compress the overstretched veins, improving the closure of the venous valves and promoting blood circulation to the heart. They keep existing venous diseases under control and prevent the development of new varicose veins. They also have an aesthetic benefit by concealing the varicose veins. Numerous studies also show that medical compression stockings significantly relieve symptoms such as feelings of heaviness or tension, pain, and swelling, thus improving quality of life.
- Natural substances: Substances like horse chestnut also have an effect on the vein wall and can be useful as part of a holistic vein therapy. Special skin care products can also support the treatment. Our tip: Applying cream directly after showering while your skin is still slightly damp allows the active ingredients to develop their beneficial properties most effectively.
- Medication supplements: Unfortunately, there are no cures for varicose veins, but certain medications can be a useful complement to therapy. Venous tonics activate the muscles in the vein wall and increase the vein's tone, which accelerates blood flow. Edema-protective medications make the vessel walls less permeable, thus preventing excessive fluid accumulation in the tissue. Both types of medications reduce the feeling of tension and heaviness in the legs and support compression therapy.
- Lifestyle changes: Certain behaviors can help prevent varicose veins or relieve the discomfort of existing varicose veins by relieving pressure on the veins and improving blood flow in the legs. It's important to avoid prolonged sitting and standing. Instead, exercise regularly. Avoid crossing your legs while sitting to avoid obstructing blood flow. Being overweight should also be avoided, as it puts additional pressure on the veins.
- Helpful exercises: Foot and ankle exercises, such as twirling your toes up and down or circling your feet, can be very helpful in relieving pressure on the veins and improving circulation. Our tip: Try elevating your legs several times a day, ideally above heart level. Gravity acts as a support in this position, allowing blood to flow more easily from the legs back to the heart. This helps reduce pressure in the veins and prevents blood from pooling in the legs.
Relieve varicose veins with acupressure
We now know that if you have varicose veins, it's important to consult a doctor early and take appropriate treatment measures. Compression stockings, regular exercise, and avoiding prolonged periods of standing or sitting can help relieve symptoms and prevent the disease from progressing.
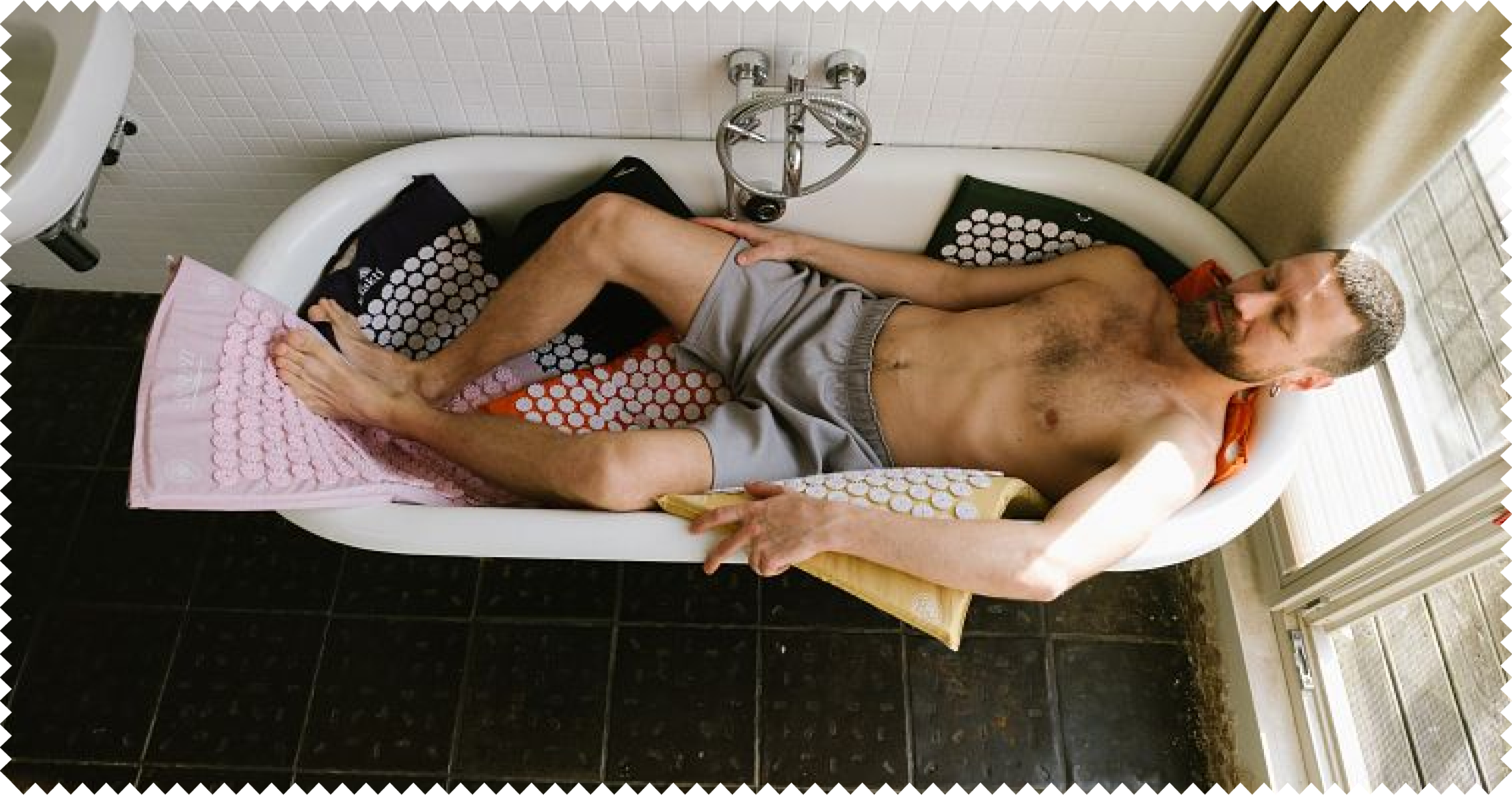
If you want to be even more active, there are suitable exercises (see above) as well as the possibility of acupressure You can even easily do this yourself at home, for example on an acupressure mat . With its numerous small spikes, it can also help relieve varicose vein symptoms by improving circulation and reducing swelling. The spikes on the mat apply pressure to specific points on the body, leading to muscle relaxation and improved circulation.
And how do I use the acupressure mat for varicose veins?
It's incredibly simple. Place the acupressure mat on a flat, comfortable surface. If you're using the acupressure mat for the first time, a thin layer of fabric (such as a towel) can help you get used to the feel of the spikes.
As a beginner , it's best to lie on a mat with lots of spikes to distribute the pressure evenly. Position yourself on the mat so that your legs are directly on the acupressure points. You can also wrap the mat around your calves or place your thighs on it. Now try to relax as much as possible and breathe deeply. Stay in this position for five to ten minutes. This time can gradually be increased to up to 30 minutes, depending on what you find most comfortable.
However, the frequency of use is definitely more important than the duration of use. Use the acupressure mat regularly, ideally daily, for optimal results. Consistency is crucial for long-term improvement of circulation and relief of varicose vein symptoms.
Our tip: While using the acupressure mat, you can also slightly raise your legs to further improve blood flow. For example, use a Pillow to raise your legs to an elevated position.
Please note, however, that if you are suffering from severe pain or significant discomfort, you should consult a doctor to receive a comprehensive diagnosis and appropriate treatment.
When is varicose vein surgery advisable?
The topic "What to do about varicose veins?" naturally includes not only the conservative methods already discussed, but also surgical interventions. If your varicose veins continue to cause pain despite compression stockings, exercises, creams, and medications, then it may be time to close the varicose veins or remove them completely. Of course, your doctor's assessment is crucial here.
Surgery is recommended when varicose veins cause severe pain, significantly impair quality of life, or pose a risk of complications such as thrombosis or ulcers. Varicose veins can be removed using various medical interventions, such as sclerotherapy, laser treatments, or surgical procedures. These methods aim to improve blood flow by closing or removing the affected veins.
- Option: Closing veins
With intravenous or endovenous therapy, the veins are sealed from the inside and remain in the body. These sealed veins then no longer transport blood. Healing is generally faster than after surgery, allowing patients to return to their usual activities sooner.
Although complications such as bruising, wound infections, or sensory disturbances can occur, these are less common than with surgical procedures. Therefore, endovenous therapy is becoming increasingly common. There are two methods of vein closure: thermal ablation and sclerotherapy.
In thermal ablation, the veins are sealed from the inside using heat, using radiofrequency or laser beams. Sclerotherapy involves injecting a fluid or foam into the vein, damaging the inner vein wall and closing it.
- Option: Removing varicose veins
During surgical interventions, the affected veins are surgically removed. Two common procedures are crossectomy (vein stripping) and phlebectomy. In crossectomy, the affected vein in the groin or back of the knee is closed and then pulled out; this is more suitable for larger veins.
Phlebectomy, also called the crochet or hook method, involves making several small incisions along the affected vein. A hook is inserted to separate the vein into sections and remove them, which is more suitable for smaller veins.
Important: These procedures can cause complications such as wound infections, bruising, and nerve or lymphatic vessel damage, and should therefore be carefully considered. Visible scars may also remain after such procedures, and new varicose veins may sometimes develop in the surrounding area. Of course, your doctor will explain the entire surgical procedure to you in detail.
This is how you can prevent varicose veins:
Finally, we'd like to return to the following question: How do varicose veins develop? Only with this knowledge can we prevent them. The German Venous League (Deutsche Venen-Liga e. V.) has developed the easy-to-remember 3L-3S rule for this: "It's better to walk and lie down than to sit and stand." Alternating contraction and relaxation of the leg muscles while walking and lying down significantly promotes venous function. Here are some tips to help you keep your venous system in good shape in your daily life:
- More exercise: Move as often as possible. Take the stairs instead of the elevator, bike instead of the car... you're probably already familiar with all the little ways to get more exercise in your daily life. If you do have to sit for extended periods, change your position regularly and put your feet up. At the office, for example, you can get up once an hour and walk around for a few minutes.
- Special exercises: Schedule ten minutes of venous exercises daily to activate your calf muscle pump. Exercises such as foot circles, heel raises, and toe rocking are particularly effective. Feel free to also try activities like swimming or cycling, which strengthen your leg muscles and promote circulation.
- Healthy diet: Eat a healthy, balanced diet. A diet rich in fiber, fruits, and vegetables supports venous function. It also helps you control your weight. Every pound you lose relieves pressure on your veins and improves blood circulation.
- Comfortable clothing and shoes: Wear mostly comfortable, loose-fitting clothing, as jeans or pants that are too tight can restrict blood flow. Also, choose comfortable, flat shoes that support your calf muscle pump. High heels may look chic, but they can restrict blood flow in your legs and should therefore be worn sparingly.
- Take a cold shower: Regularly shower your legs with cold water. The cold water causes the veins to constrict, improving blood flow to the heart. Start at your feet and slowly work your way up to your buttocks.
- Avoid heat: If possible, avoid hot baths, underfloor heating, and saunas. Warm temperatures cause veins to expand, making it difficult for blood to return to the body. If you do want to visit a sauna occasionally, you should rinse your legs with cold water afterward.