The diagnosis of cervical spine syndrome is not so easy. Patients often drag themselves from one doctor to another, taking strong painkillers, but hardly achieving any relief from their symptoms. It pulls in the neck, turning the head causes pain and sometimes this radiates into the arms. This is anything but pleasant. The cervical vertebrae support the head, the center of our nervous system - so it is correspondingly bad for patients when this part of the body goes on strike. What alternatives are there to medication, and how can acupressure help to finally get the head spinning freely again? Below, we explain exactly what the causes and symptoms of a cervical spine blockage are and what treatment options are available.
Content
1. acupressure for cervical spine syndrome: Far Eastern traditional medicine for neck and back pain
2 What exactly is cervical spine syndrome?
3. the symptoms of cervical spine syndrome
4. causes and duration of cervical spine syndrome
5. the diagnosis of cervical spine syndrome
6. treatment of cervical spine syndrome
7. acupressure as a therapeutic approach for cervical spine syndrome
8. cervical spine syndrome: multicausal origin, multimodal treatment
Acupressure for cervical spine syndrome: Far Eastern traditional medicine for neck and back pain
Acupressure is a form of acupuncture and goes back to the methods of traditional Chinese medicine. The treatment is based on the knowledge that pain relief is possible when certain energy blockages in the body are released. In acupressure, this is achieved either with finger pressure or with specially made acupressure mats, which are reminiscent of the nail boards used by fakirs or yogis in India.
Neck and shoulder tension can have a wide variety of causes, e.g. a cervical spine distortion (whiplash injury) or a slipped disc.
In the treatment of cervical spine, scientific studies such as the 2016 study by the University of Munich and others (Dägfa overview of the study situation for acupuncture) assume that treatment with acupuncture has a positive effect. How can this correlation be explained?
What exactly is cervical spine syndrome?
The cervical spine consists of seven vertebrae (upper = 1 and 2, middle = 3, 4, 5, lower = 6 and 7). These support the head and are susceptible to tension and pain due to their structure and fine mechanics. All complaints relating to the cervical spine are referred to as cervical spine syndrome. It is usually associated with restricted movement in the shoulder and neck area, sometimes the pain also extends into the arms.
The structure of the cervical spine
The seven cervical vertebrae are each separated by an intervertebral disc. It functions like a shock absorber and cushions sudden movements. As the upper end of the spine, the cervical spine has to perform important tasks such as tilting and turning the head, as well as stretching and bending the upper back. The vertebrae are naturally held and supported by the cervical muscles that surround them.
If something goes wrong, this can lead to a herniated cervical disc, for example, or certain muscle strands around the vertebrae stiffen and form a blockage. We refer to this as cervical spine syndrome or cervical syndrome.
Acute or chronic cervical spine syndrome
Doctors differentiate between cervical spine syndrome not only according to where it occurs (1st-7th vertebrae), but also according to the duration of the symptoms. If it lasts for more than three months, it is referred to as chronic cervical spine syndrome. Those affected are already familiar with the clinical picture and often suffer from recurring pain in the shoulder and neck area.
Acute cervical spine syndrome is different: it is caused by sudden overuse (1st-3rd week: acute, 4th-12th week: subacute). Typical causes would be neck pain after gardening or an injury such as cervical spine distortion, whiplash, which occurs in a traffic accident.
The symptoms of cervical spine syndrome
The symptoms of cervical spine syndrome vary depending on which vertebrae they are located on and what triggered them. In addition, there are physical signs of wear and tear, which have an increasing influence on the course of the symptoms with increasing age.
Nevertheless, there are some typical symptoms of cervical spine syndrome:
- Stiffening of the neck
- Pulling and burning in the neck and shoulder muscles
- Limited mobility of the head
- Headache
- Migraine attacks
- Tinnitus
- Dizziness
- Visual disturbances
- Nausea
- Pain radiating to the shoulders and arms
- Tingling or numbness in the hands
If the symptoms remain untreated or are misdiagnosed, they can increase and become chronic. Therefore, affected persons should consult a physician in time, also to exclude neurological diseases with similar symptoms.
Causes and duration of cervical spine syndrome
The cause of a cervical spine syndrome is not always as obvious as in the case of an accident that results in a cervical spine distortion.
Possible triggers of cervical spine syndrome:
- Stress and lack of exercise: People who sit in an office for long periods of time or spend a lot of time in a one-sided posture are more susceptible to cervical spine syndrome than people who exercise every day. Initially, tension develops, which then leads to hardening of the neck muscles. Purely psychological causes such as high levels of stress usually make the diagnosis more difficult.
- Injuries and accidents: The pain can be explained by sudden external impact on the affected person's muscles and vertebrae. For example, a whiplash injury or the affected person has lifted a heavy object awkwardly.
- Age-related wear and tear: The vertebrae, supporting ligaments and intervertebral discs in particular degenerate over the course of our lives; they become less supple and therefore offer less support in the event of unexpected movements of the neck or back.
- Joint blockages: A cervical spine blockage restricts mobility from one moment to the next. The pain usually radiates, the affected person feels like they have lumbago, only the blockage is higher up on the spine.
- Inflammations: Each vertebra has its own vertebral arch or facet joints. If these become inflamed, facet syndrome occurs. This clinical picture is sometimes triggered by bacteria, but often also by overuse, e.g. by carrying heavy objects.
- Side effect of other pre-existing conditions: People suffering from osteoporosis or rheumatism often also develop cervical spine syndrome. Patients who are being treated for tumors or scoliosis can also suffer from complaints relating to the cervical vertebral muscles.
How long does the cervical spine syndrome last?
We already know the distinction between acute, subacute and chronic cervical spine syndrome. Accordingly, the answer to the question is how long the symptoms last: Unfortunately, this can vary greatly. It is important that the diagnosis is made quickly and the cause of the pain is found. If this is the case, it may be possible to prevent the disease from becoming chronic. If the cervical spine syndrome has a psychological cause, this can perhaps be remedied; if it is an inflammation or a blockage, patience is required. Without treatment and personal initiative, e.g. acupressure by a Shakti Mat, it is highly likely that the condition will become severe.
The diagnosis of cervical spine syndrome
The difficulty in diagnosing cervical spine syndrome lies in the fact that many inconsistent symptoms occur simultaneously. Anyone suffering from discomfort in the neck and shoulder area should consult a doctor.
In practice, the diagnosis is carried out as follows:
- Medical history: The doctor asks the patient about the symptoms and the course of the illness. It is worth considering in advance how you can best describe your own pain and also share ideas for possible other causes or concerns with the doctor.
- Examination: The doctor performs a physical examination of the patient to determine where the pain points are located. He looks for inflammatory reactions and misalignments and palpates the affected person in the tense regions.
- MRI: In individual cases, the doctor may order a magnetic resonance imaging scan. This allows him to rule out, for example, a slipped disc as the cause of the cervical spine syndrome or another acute injury.
- Diagnosis: Acute or chronic? Has the cause of the cervical spine syndrome already been determined? Depending on the clinical picture, the doctor will decide on further treatment after diagnosis.
Treatment of cervical spine syndrome
No one in medicine has believed for a long time that back pain can be permanently relieved by medication alone. The treatment of cervical spine syndrome usually involves several approaches - both with the active participation of the patient and with passive forms of therapy. Experience has shown that a combination of different treatment approaches leads to success.
What methods are used here?
Drug therapy
Painkillers are not a solution, but they can offer a bridge to new possibilities. As painkillers loosen the affected muscle area and relieve inflammation, they are usually first aid in times of need.
However, this mainly applies to acute cervical spine syndromes; treatment with medication is problematic for long-term pain. Side effects can occur and dependencies can develop that further impair the patient.
Physiotherapy
Exercise is an important component in the healing process for cervical spine syndrome. The tension around the neck muscles can be reduced by exercising the upper body. A physiotherapist works to utilize the natural tensile forces of the muscles and to equalize the strain on a specific point in the nerve or muscle area. Stretching exercises or exercises with fascia rolls, for example, can be useful measures for cervical spine syndrome. The advantage of this form of therapy is that those affected can continue the exercises at home and thus actively participate in the healing process themselves.
With the help of your acupressure mat, you can prepare your muscles even better for a massage treatment, as physiotherapist Anne confirms in the following video:
Herbal medicine
Purely herbal medicines can also provide some pain relief. These preparations are usually based on essential oils that can help to relax muscles and reduce inflammation, e.g. eucalyptus, pine or spruce needles. The tinctures are obtained from plant parts such as roots, bark or flowers, e.g. from arnica, yarrow or calendula.
Electrotherapy and physical therapy
These two methods can complement other treatments. For example, a hot bath, a sauna session or a shoulder-arm wrap have a pain-relieving effect for many patients. Of course, massages can also have a positive effect as long as they are performed by recognized physiotherapists. Electrotherapy works with ultrasound, red light, but also iontophoresis or NSM. Both of the latter stimulate the nerves with electronic impulses.
Quaddle therapy and MIT (minimally invasive injection therapy)
Both of these are therapeutic approaches for chronic pain patients. Wheal therapy is controversial. Small amounts of an anesthetic are used to relax the muscles and block the pain stimuli. MIT is mainly suitable for patients with symptoms of paralysis. A combination of injected painkillers and external therapy methods is the last resort before an impending operation.
Operation
Surgery under general anesthesia is what patients with cervical spine syndrome want to avoid. It is used when all treatment methods have failed. Such a step is usually considered after three months of treatment. In the past, the surgeon used to approach the cervical vertebrae via an incision in the rib cage, whereas today it is done via the patient's neck. Cervical spine operations involve numerous risks and should therefore only be performed in extreme emergencies, e.g. if the replacement of an intervertebral disc is unavoidable.
Acupressure as a therapeutic approach for cervical spine syndrome
Pain specialists have long pointed out that acupressure can lead to pain relief. By applying pressure to certain parts of the body, the muscles relax and the patient experiences possible relief. Acupressure is a form of acupuncture and has a long tradition in the medical history of Asia. It is applied either with a gentle pressure massage by a therapist or with external aids such as an acupressure cushion or an acupressure mat.
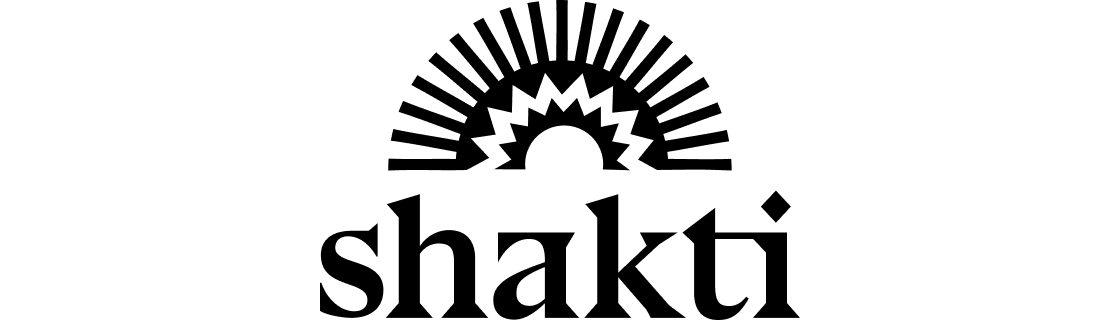
The Shakti Mat and the Shakti Pillow offer cervical spine syndrome sufferers a good supplement to conventional pain therapies. Those affected normally use them for around 20 minutes: They roll the acupressure mat into a Pillow and place their neck on it. As the Shakti Mat promotes blood circulation in a similar way to an Indian nail cushion, many sufferers find the first encounter challenging. The body first has to slowly get used to the spikes in the neck and shoulder area. However, this usually happens within 21 days.
The effect of acupressure on cervical spine syndrome
Curious how these little spikes can help you?
When acupressure is applied, the body releases endorphins and after a few minutes, a feeling of warmth develops in the painful area. Patients report that their headaches and migraines subside and their tension is immediately relieved. Fascia and muscles relax and the healing process can begin. The acupressure mat can also be used for the entire back and neck area. Those affected usually integrate the application into their daily routine and, for example, make an evening ritual of relaxing on the Shakti Mat for a few quiet minutes.
Some exercises for a pain-free everyday life
Mobility
Gradual mobilization is the best way to gently restore mobility to the neck. You can do this exercise three times a day:
Turn your head as far to the right as you can and nod a few times. Now slowly turn your head to the left and nod here too. It is important that your back remains completely straight. Then tilt your chin up to your chest. Lower your head as far as you can and then slowly turn it from one side to the other. For the third exercise, push your head far forward. Make a long neck. Then pull your head back in as if you wanted to make a double chin. Over time, you will notice how these movements become easier and easier.
Strengthening
As well as improving the mobility of your neck, you should also strengthen its muscles. There is a simple and effective exercise for this too:
Place your hand on your forehead and stretch your neck. Now press your head against your hand for 10 seconds and then relax again. Repeat this tension a few times. You can do the same with your hand on your temple. Of course, press your head against the hand on the side of your temple. Do this at least once on each side. Again, it is important to keep your back as straight as possible during the exercise.
The wonderful yoga teacher Nico shows you more exercises with the Shakti Mat especially for the neck in our video:
Cervical spine syndrome: multicausal origin, multimodal treatment
People who suffer from tension in the neck muscles and cervical vertebrae are severely restricted in their everyday lives. Pain always has a psychological impact, it makes people uncomfortable and causes them to withdraw. With targeted therapy methods, patients can break out of the acute pain and prevent the cervical spine syndrome from becoming a chronic burden.
Depending on the individual case, treatment should include a combination of physiotherapy, medication, special pain-relieving therapies and acupressure. It is best for the individual to find out for themselves what is good for them. If the diagnosis is made quickly and the therapy is effective, surgery is not necessary in most cases. However, triggers (such as stress) may need to be eliminated and new approaches to pain relief may need to be explored.
If you would like to discuss the topics of acupressure and acupressure mats with cervical spine syndrome, give other people tips or ask questions, you are very welcome to join our large Facebook community.
Sources
- Dr. Gumpert, Nicolas: Acute cervical spine syndrome, 2020 via https://www.dr-gumpert.de/html/akutes_hws_syndrom.html
- Dr. Gumpert, Nicolas: Chronic cervical spine syndrome, 2020 via https://www.dr-gumpert.de/html/chronisches_hws_syndrom.html
- Dr. Gumpert, Nicolas: Cervical spine syndrome, 2020 via https://www.dr-gumpert.de/html/hws_syndrom.html
- Dr. Lemberger, Matthias: Cervical spine surgery, 2020 via https://www.qualitaetskliniken.de/behandlungen/hws-op/
- Dr. Köstler, Paul: Cervical spine syndrome via http://www.drkoestler.at/cervikal-hws/
- Dr. Sagstetter and colleagues: Minimally invasive spinal treatment via http://www.orthopaedie-landshut.de/behandlung-konservativ/minimalinvasive-wirbensaeulentherapie.html
- Fleckenstein, J., Stör, J., Stör, W.: The study situation on the effect of acupuncture on pain in the cervical, thoracic and lumbar spine, in "Wissenschaft für die Kitteltasche", 2016
- Ganepour, Bijan/ PD Dr. med. Kubosch, David-Christopher: Cervical spine syndrome: pain in the cervical spine, via https://gelenk-klinik.de/wirbelsaeule/hws-syndrom-beschwerden-halswirbelsaeule.html
- Liebscher-Bracht, Roland: Cervical Spine Syndrome (HWS-Syndrom) - What is really behind the embarrassing diagnosis? via https://www.liebscher-bracht.com/schmerzlexikon/hws-syndrome/
- Stollberg, Carolin: Cervical spine syndrome: symptoms, causes and treatment, 2019 via https://www.ratgeber-nerven.de/rueckenschmerzen/haeufige-arten/hws-syndrom/
- Wu, Lilli: Acupuncture in the treatment of cervical spine syndrome, A multi-method approach for an intercultural comparison between China, Germany and Argentina, Medical Faculty of the Ludwig-Maximilians-University Munich, 2016