Are you sometimes plagued by a stiff neck or pressing back pain after a long day at your desk? These everyday aches and pains, which we usually carelessly ignore, can be caused by a widespread and often underestimated condition: osteochondrosis. This is a degenerative disease of the spine that affects millions of people worldwide and can cause a variety of symptoms - from back pain and stiffness to numbness and muscle weakness. But what is behind this condition that affects the daily lives of so many? Let's take a closer look together at its causes, symptoms and treatment options. With this knowledge, we will then show you effective exercises that can alleviate the symptoms and improve your quality of life.
Content
2. in focus: osteochondrosis of the spine
3. common osteochondrosis symptoms
4 What to do with osteochondrosis?
5. osteochondrosis exercises that can help
6. osteochondrosis - lumbar spine exercises for your everyday life
What is osteochondrosis?
First, let's establish a basis with an understandable definition of osteochondrosis: this is a disease that primarily affects the joints - especially those of the spine. It occurs when the cartilage tissue that normally protects the joints and makes them flexible wears down or degenerates. This leads to a change in the structure and function of the affected joints.
There are several factors that can contribute to the development of osteochondrosis, including genetic predisposition, ageing, repetitive strain or injury to the affected joints. Unhealthy lifestyle habits with a lack of exercise and a poor diet are also not to be neglected as causes. The symptoms of osteochondrosis can vary depending on the joint affected. There is often pain in the joint area, stiffness, restricted mobility, muscle tension and sometimes also numbness or tingling. In advanced cases, this can of course also lead to a considerable restriction of everyday activities. At the latest then, and preferably at an early stage, you should start appropriate treatment. This is usually aimed at alleviating the symptoms, improving mobility and slowing down the progression of the disease.
Treatment options include physical therapy to strengthen the muscles and improve mobility, pain medication to relieve discomfort, injections of anti-inflammatory drugs to reduce inflammation and, in some cases, surgical procedures such as the removal of damaged tissue. Although the disease cannot always be completely prevented, some measures can reduce the risk. These include regular physical activity to strengthen muscles and maintain flexibility, a balanced diet to promote bone and cartilage health, avoiding excessive strain on joints and maintaining correct posture when sitting, standing and lifting heavy objects. So much for a brief introduction to the topic. Now let's look at the details - and then, of course, the appropriate exercises.
What are erosive and activated osteochondrosis?
Erosive osteochondrosis is a special form in which there is increased cartilage degradation and erosion of the bone surface. In contrast to the typical course, in which the degenerative changes mainly affect the cartilage and the intervertebral discs, the erosive variant leads to additional damage to the adjacent bone structures. Similar to general osteochondrosis, factors such as ageing, genetic predisposition, overloading of the joints and injuries play a role. Inflammatory processes can also occur. The symptoms of the erosive form are also often similar to those of the conventional form. In advanced cases, however, bony deformities and joint destruction can also develop, which can lead to even greater discomfort and impairment.
In the case of activated osteochondrosis, severe pain or a noticeable worsening of the usual symptoms suddenly occurs. In this context, activated means that the existing disease is acutely exacerbated by external influences or stress. These can be injuries or trauma, but also excessive strain on the affected joints. A slipped disc, a pulled muscle or incorrect movement, for example, can lead to this. All people with osteochondrosis should therefore be aware that it can also occur as activated osteochondrosis. They can then act appropriately if the worst comes to the worst and take suitable first aid measures, such as immediate rest, cooling and pain relief. Regular exercise, good posture and avoiding heavy strain on the affected joints are suitable preventative measures.

In focus: Osteochondrosis of the spine
Osteochondrosis of the spine, also known as spondylosis or spondylarthrosis, affects the intervertebral discs and vertebral joints of the spine. It can occur, for example, as osteochondrosis of the cervical spine (in the cervical spine) and as osteochondrosis of the thoracic spine (in the thoracic spine). To understand this in more detail, the spine consists of a series of vertebrae separated by intervertebral discs. These intervertebral discs consist of an outer fibrous layer and a gel-like core. The vertebral joints are formed by the facet joints, which are located between the adjacent vertebrae.
The disease of the spine often manifests itself in back pain, which can be aggravated by movement or exertion and which subsides during periods of rest. It can also lead to stiffness, limited mobility and muscle tension in the affected area.
Unlike other forms that focus on specific joints such as the knee, hip or shoulder, spinal disease specifically affects the structures of the spine, particularly the intervertebral discs and facet joints. It therefore has a much broader effect on your musculoskeletal system. The symptoms and treatment options can therefore also differ from other forms, as the stress and functioning of the spine is unique compared to other joints. Below we explain a few suitable exercises that you can easily integrate into your everyday life.
Common osteochondrosis symptoms
At the very beginning, we briefly discussed the symptoms associated with the disease. Now we would like to explain in detail which (initial) signs may indicate osteochondrosis. Back pain is one of the most common symptoms of osteochondrosis of the lumbar spine. This pain can feel different - from dull and pressing to sharp and stabbing. It can also worsen when you perform certain movements or remain in a certain position for a long time. An example from everyday life would be the onset of back pain after a long day at the office, especially if you have been sitting at your desk in a bad posture.
The disease can manifest itself through stiffness and limited mobility of the spine, especially in osteochondrosis of the cervical spine. Symptoms can also vary significantly depending on the degree of severity, for example the feeling of immobility when getting up in the morning. The degenerative changes in the spine can also cause the surrounding muscles to attempt to stabilize the unstable areas, which can lead to muscle tension. This may cause additional pain and discomfort. As a result, in some cases, pain can radiate from the affected area to other areas of the body. This can ultimately lead to your everyday life being made more difficult by (more or less) restricted activities. Movements such as bending, lifting or walking can only be carried out with great difficulty and pain. This naturally results in a considerable reduction in quality of life and independence.
What to do with osteochondrosis?
The causes of osteochondrosis can be varied and are often the result of a combination of genetic, lifestyle, ageing and environmental factors. We can tackle some of them directly in order to achieve an improvement or carry out effective prevention. Others, unfortunately, we cannot influence. Genetic predisposition can play a role in development. Certain genetic variations can affect the structure and function of cartilage and bone tissue, which can increase the risk of degenerative changes. People with a family history may have a higher risk of developing the condition. Although you cannot influence this, you can monitor it closely so that you can act in good time. The situation is similar with the ageing process. With increasing age, the elasticity and flexibility of cartilage tissue decreases, which can lead to an increased risk of degenerative changes.
Preventive measures
Now we come to the risk factors that you can (at least partially) influence. Excessive strain and repetitive stress on the joints in particular can contribute to the wear and tear of cartilage tissue. This can of course be encouraged by certain occupations or activities. Jobs or hobbies that involve heavy lifting, an unhealthy posture or repeated impact loads are examples of this. Of course, you cannot always avoid these, but you can always ensure effective compensation (rest and suitable exercises for osteochondrosis of the cervical spine, thoracic spine or lumbar spine). Acute injuries or trauma, such as falls, accidents or sports injuries, can also lead to damage to the intervertebral discs and joints, which can promote the development of osteochondrosis in the long term. You cannot always influence this either. However, a little mindfulness, especially during sport, can perhaps prevent one or two injuries.
What you can also avoid most of the time: Being overweight and obese. Excessive body weight can put additional pressure and strain on the joints - especially the weight-bearing joints such as the spine. This can accelerate the breakdown of cartilage tissue and increase the risk. Smoking and unhealthy lifestyle habits such as an unbalanced diet and lack of exercise also increase the risk of degenerative changes. Smoking, for example, can restrict blood circulation and thus impair the supply of nutrients to the joints, which can promote the breakdown of cartilage tissue. Conclusion: Prevention should include a combination of healthy lifestyle habits, regular physical activity to strengthen and mobilize, muscle relaxation, weight management and avoidance of excessive stress on the joints.

Osteochondrosis exercises that can help
Now you're probably asking yourself: What can you do about osteochondrosis? We are happy to go into this in more detail. We have just learned that regular and gentle exercise helps in the treatment of osteochondrosis and is therefore an integral part of osteochondrosis therapy. Certain exercises can help to alleviate symptoms, improve mobility and strengthen the muscles, whether the disease is already present or is developing. A combination of stretching exercises, trunk-stabilizing workouts, mobilizing exercises, general fitness training and muscle relaxation has proven effective. This five-set approach is suitable for cervical spine osteochondrosis exercises as well as for osteochondrosis of the thoracic or lumbar spine.
We have put together some exercises that can help with osteochondrosis of the spine, especially lumbar spine osteochondrosis. Please perform these exercises slowly and in a controlled manner and stop immediately if you feel pain or discomfort. You can of course also consult a physiotherapist or doctor.
Osteochondrosis - lumbar spine exercises for your everyday life
- Stretching: Gentle stretching exercises can help to improve the flexibility of the lumbar spine and reduce stiffness. One example of this is the cat-camel stretch. You start it in a quadruped position, then arch your back upwards and then pull your stomach in (cat hump). Then lower your back down and raise your head and buttocks slightly (camel hump). Perform this movement slowly and in a controlled manner and repeat it several times as you feel comfortable.
- Stabilization: Now we strengthen the muscles in the lower back and buttocks. Again, start in a quadruped position. From this position, alternately lift one leg backwards and upwards - keeping your back straight. Hold your leg in the air for a few seconds and then carefully lower it. Repeat the exercise with the other leg. In addition, exercises that strengthen the muscles in the middle and upper torso area contribute to an overall stable spine, which in turn can relieve pain. This includes, for example, the classic forearm support, also known today as the plank.
- Mobilization: Exercises to increase mobility in the spine can also help the intervertebral discs to adapt better, reduce restricted movement and also reduce pain. Examples of this are spinal rotations and side bends. Please always perform these slowly and evenly.
- Fitness: Aerobic exercises such as walking, swimming or cycling improve general fitness, promote blood circulation and can therefore relieve pain. However, it is important that these exercises do not put additional strain on the affected joints. Swimming is therefore definitely the right choice for knee problems, as well as for back pain.
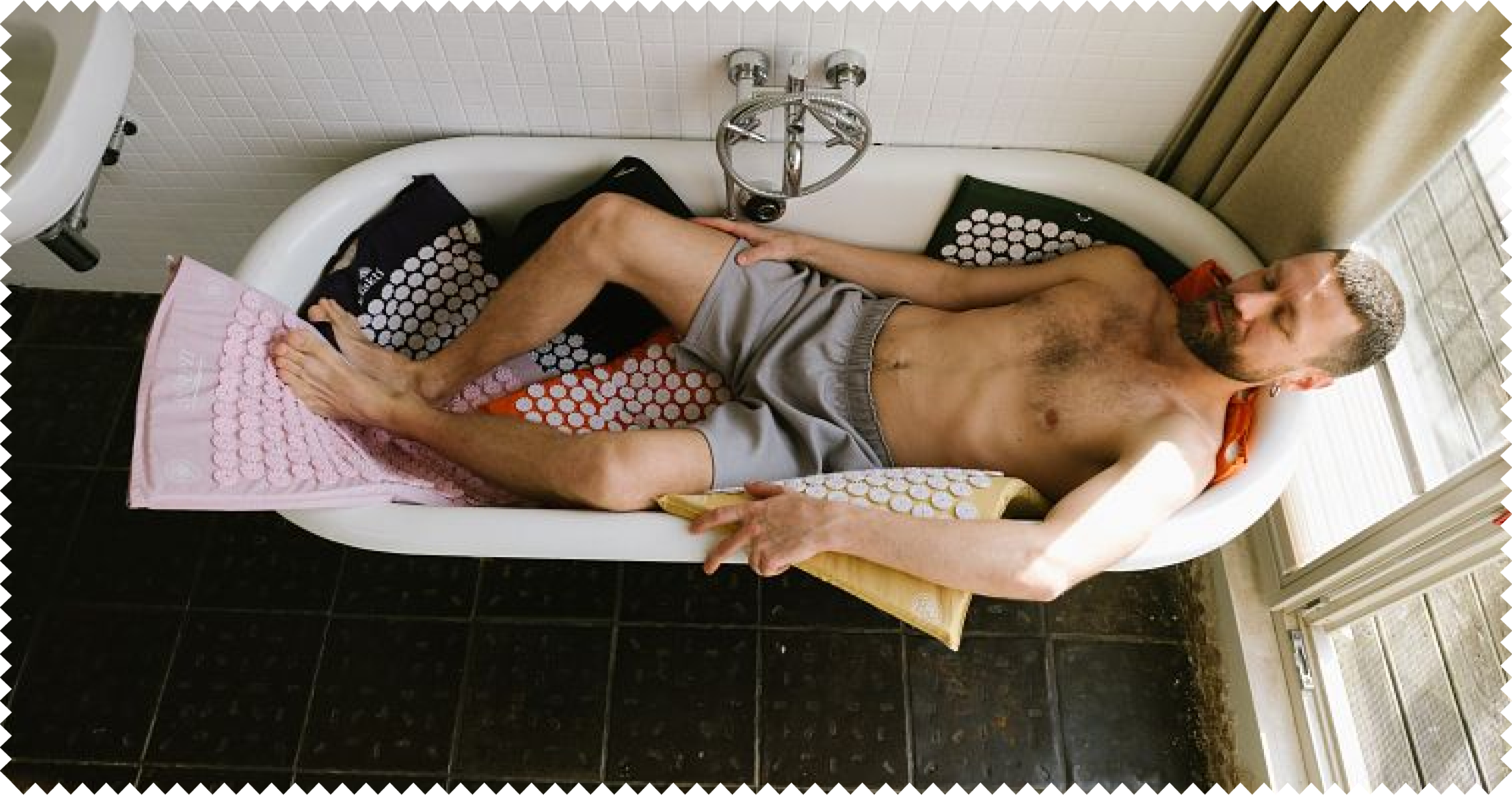
- Muscle relaxation: After you have stretched, strengthened and mobilized your muscles, they can now relax. This is particularly easy on an acupressure mat. Simply lie down on it and let the spikes stimulate your circulation and relax your muscles. Our tip: Beginners are best off starting on a mat with as many spikes as possible, while advanced practitioners relax very well on a mat with fewer spikes. Try it out and enjoy a pleasantly liberated feeling after just a few minutes!